FDA-Approved RSV Vaccine Enabled by Work of UT Molecular Biologist
Every year, millions of people become sickened by RSV, and more than 100,000 die. New vaccines with a connection to UT Austin may help turn those numbers around.
The first-ever vaccine approved by the FDA to treat RSV was made possible by research from UT Austin molecular biologist Jason McLellan and others.
The first-ever vaccines approved by the Food and Drug Administration and its team of advisers to treat respiratory syncytial virus (RSV) use research by a scientific collaboration that includes Jason McLellan, a professor of molecular biosciences at The University of Texas at Austin.
“This is one of the most important viral pathogens for which we still lacked a vaccine. This milestone also means a lot to me and Barney Graham,” said McLellan, referring to a colleague he worked with at the National Institutes of Health where McLellan was a postdoctoral scientist at the time. “This is the first example where we got structure-based vaccine design to work.”
People contract RSV in all stages of life, but it’s most dangerous in the young and the old. The virus causes pneumonia, bronchiolitis and other diseases of the lower respiratory tract. Every year, millions of people become sick with RSV, and more than 100,000 die, mostly in areas that lack access to modern medical care. For infants under one year of age, RSV is second only to malaria for infectious disease deaths.
Scientists have searched for decades for an effective vaccine. McLellan, Graham and Peter Kwong of the National Institute of Allergy and Infectious Diseases’ Vaccine Research Center showed in 2013 that a then-new approach, called structure-based vaccine design, could lead to an effective RSV vaccine. McLellan, Graham and others later used the same approach to design a key element of the FDA-approved COVID-19 vaccines.
It was already known that a certain part of RSV, called the F protein, is responsible for infection. But the F protein is a shape shifter — before it infects and fuses with a cell, its shape (what scientists call its “presfusion conformation”) is different from after it enters the cell. If the immune system encounters an RSV virus with the F protein in this prefusion shape, it makes potent antibodies. But in its postfusion conformation, the antibody response is weak and, therefore, not suitable for a vaccine.
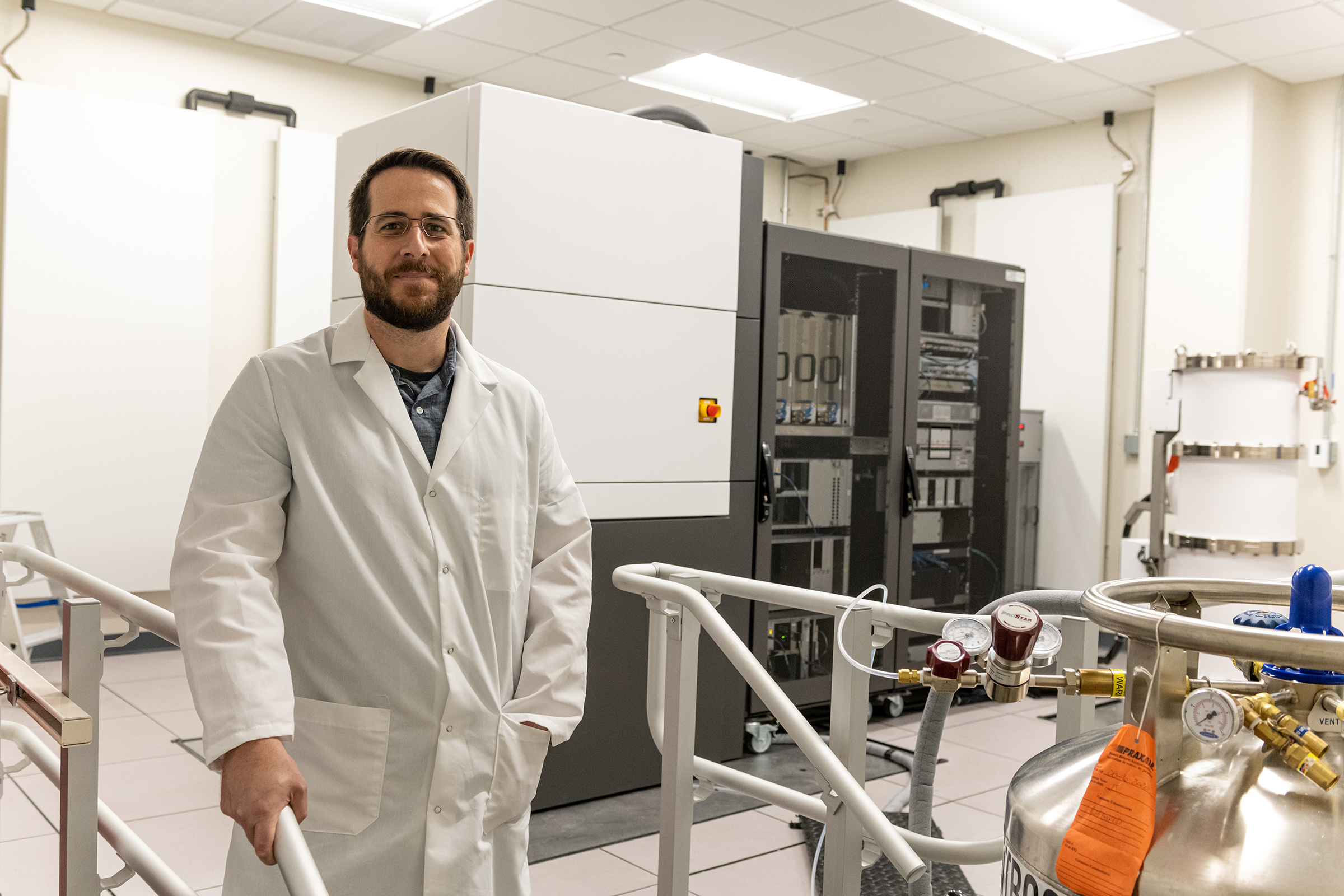
This is where the structure-based approach comes in. First, McLellan and the team used a technique called X-ray crystallography to determine the atomic-level structure of the F protein. Next, they developed ways to keep the F protein from shape-shifting, locking it in the conformation that elicits the right antibodies.
In 2013 the team tested several versions as a vaccine in both mice and nonhuman primates. These protein variants elicited high levels of neutralizing antibodies and protected the animals against RSV infection.
“Our first time testing these stabilized molecules in animals, the response was 10-fold higher than anything anyone had ever seen before,” said McLellan, who holds the Robert A. Welch Chair in Chemistry. “And at that point, we’re thinking, ‘This is it. We’ve got it.’ That was exciting.”
Approved on May 3, GSK’s vaccine Arexvy showed a 94% reduction in severe illness and was nearly 83% effective against lower respiratory tract illness in human trials; it was recommended in March for approval by an advisory committee to the FDA. Based on the work by McLellan, Graham and Kwong at the NIH, Arexvy contains a recombinant subunit prefusion version of RSV F and was approved for use in older adults.
A second RSV vaccine — developed by pharmaceutical company Pfizer — also contains a stabilized, prefusion F protein based on the lessons from the research team. An interim analysis last summer showed the vaccine was roughly 86% effective against severe RSV disease. FDA advisers in May backed its use for pregnant mothers, since vaccines for that population were also reportedly shown to be safe and effective. With the pregnant patient population, the goal is to protect vulnerable infants through the natural transfer of antibodies from mother to child.
Even though COVID-19 vaccines were FDA-approved before the first RSV vaccine, work that began over a decade ago on a structure-based vaccine for RSV helped speed up the development of the first COVID-19 vaccines. Promising results in early trials of an RSV vaccine inspired McLellan to tackle vaccines for two coronaviruses that preceded COVID-19—SARS and MERS.
“Our approach to coronavirus was essentially do everything we just did for RSV,” McLellan said. “We got the structure of a coronavirus spike, figured out how to use that structure to design stabilizing mutations and then used that as the vaccine antigen. And we had that all done by around 2017. So all the coronavirus work was absolutely inspired by RSV. And RSV just provided the template for how we—and others now—approach structure-based vaccine design for many different pathogens.”
Insights from the work on RSV, SARS and MERS vaccines enabled McLellan and his collaborators to develop a structure-based COVID-19 vaccine antigen rapidly, and all of the FDA-approved COVID-19 vaccines use this antigen.
“Structure-based vaccine design is an extremely powerful paradigm for vaccine development,” said McLellan. “It’s focused on trying to engineer the best possible antigen using structural information. And you’re just seeing a huge investment in that, and a lot of vaccine manufacturers purchasing cryo-electron microscopes, hiring structural biologists and protein engineers. So it’s clearly being recognized as an important tool that’s needed for vaccine development.”
Update: This post was originally published May 3 and updated after FDA advisers backed a second RSV vaccine from Pfizer for pregnant women to help protect their newborns.
The University of Texas at Austin is committed to transparency and disclosure of all potential conflicts of interest. The University investigator involved in this research, Jason McLellan, has submitted required financial disclosure forms with the University. McLellan is an inventor on several patent applications related to this research filed by the National Institutes of Health, from which he is receiving royalties.
Share
Department of Molecular Biosciences


